Compartment syndrome is a serious condition in which pressure builds up inside a closed muscle compartment. This increased tissue pressure can reduce blood flow, depriving muscles and nerves of oxygen. Without treatment, it can lead to nerve damage, permanent muscle loss, or even amputation.
It can develop suddenly after trauma or slowly with overuse. Whether you’re an athlete, a clinician, or recovering from surgery, knowing the signs of compartment syndrome can make the difference between full recovery and long-term disability.
What Is Compartment Syndrome?
Muscles, nerves, and blood vessels are grouped into compartments, each wrapped in a tough, inflexible layer of fascia. These compartments are found in the lower leg, forearm, thigh, buttocks, hands, feet, and abdomen.
When swelling, bleeding, or fluid builds inside a compartment, the fascia can’t stretch to accommodate it. The pressure rises, blocking circulation and damaging tissues. If the compartment pressure remains elevated, tissue ischemia, nerve damage, and tissue death can occur.
Types and Causes
When swelling, bleeding, or fluid builds inside a compartment, the fascia can’t stretch to accommodate it. The pressure rises, blocking circulation and damaging tissues. If the compartment pressure remains elevated, tissue ischemia, nerve damage, and tissue death can occur.
Acute Compartment Syndrome
This is the most severe and fast-moving type. It typically develops in the lower leg, thigh, or forearm after trauma and is considered a medical emergency.
Common causes include:
- Bone fractures (especially tibial shaft fractures)
- Crush injuries or deep bruises
- Tight casts or bandages
- Vascular injury during surgery
- Prolonged pressure from immobility
- Anabolic steroid use
Without rapid treatment, acute compartment syndrome can result in permanent loss of limb function.
Chronic Exertional Compartment Syndrome (CECS)
Also known as chronic compartment syndrome, this form develops gradually from repeated physical stress. It often affects athletes and military service members, especially in the anterior compartment of the lower leg or thigh.
Causes include:
- Long-distance running
- High-repetition strength training
- Eccentric exercises (resistance while muscles lengthen)
Symptoms flare up during activity and subside with rest. Although not life-threatening, CECS can significantly impact performance if left unaddressed.
Abdominal Compartment Syndrome
This life-threatening condition occurs in critically ill patients, usually after trauma, abdominal surgery, or liver transplant. As pressure increases in the abdomen, it compromises blood flow to organs like the kidneys and intestines.
Causes include:
- Severe internal bleeding
- Fluid accumulation (ascites)
- Sepsis or infection
- Pelvic fractures or burns
This type of compartment syndrome is typically diagnosed and treated in intensive care.
Recognizing Symptoms
The symptoms of compartment syndrome depend on the type, but pain that seems excessive for the injury is often the first warning sign. For a deeper breakdown of symptoms and risk factors, WebMD’s guide to compartment syndrome offers a helpful overview.
Acute signs may include:
- Severe pain that doesn’t improve with elevation or medication
- Swelling, tightness, or bruising in the affected limb
- Numbness or tingling
- Pain when stretching the involved muscles
- Pale, shiny skin or weak pulse
Chronic symptoms can include:
- Aching, cramping, or tightness during activity
- Symptoms ease within 30 minutes of rest
- Weakness, numbness, or foot drop
- Muscle bulging during exercise
Abdominal signs may involve:
- A firm, distended abdomen
- Decreased urine output
- Low diastolic blood pressure
- Difficulty ventilating or signs of organ dysfunction
Diagnosis and Pressure Monitoring
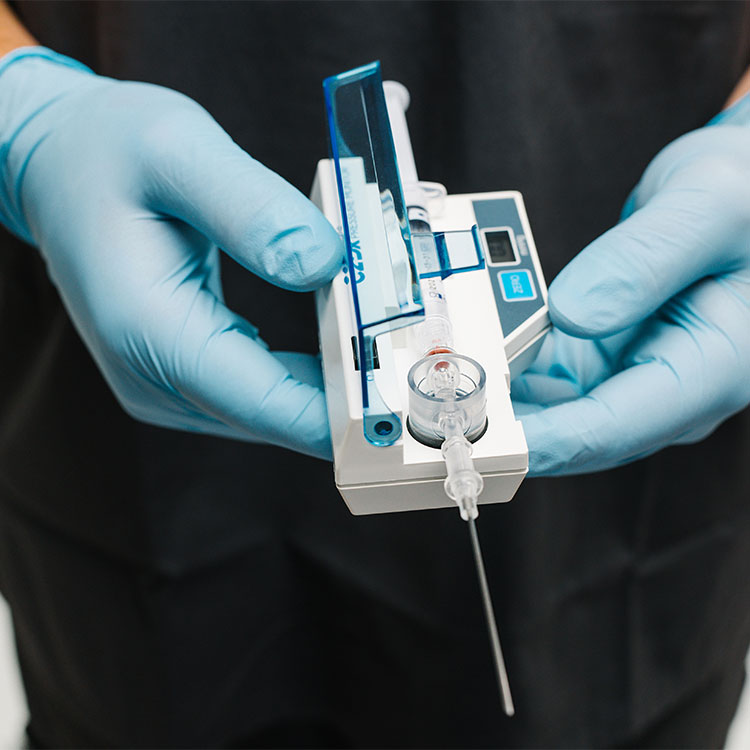
To diagnose compartment syndrome, doctors assess symptoms and perform a physical exam. The most reliable method is direct pressure measurement, which involves inserting a needle or catheter into the affected compartment. In chronic cases, measurements may be taken before and after exercise. For abdominal compartment syndrome, bladder pressure is often used as a proxy.
Other tests, such as imaging or laboratory work, may be used, but they cannot confirm the diagnosis on their own.
Treatment Options
Acute cases require immediate surgical treatment. A fasciotomy is performed to open the fascia and relieve pressure, preventing further damage. Supportive care may include IV fluids, oxygen, and removal of any restrictive devices.
Chronic cases may respond to:
- Physical therapy and activity modification
- Anti-inflammatory medications
- Orthotics
- Elective fasciotomy if symptoms interfere with daily life
The Role of STIC® Pressure Monitoring
When symptoms of compartment syndrome are unclear or progressing rapidly, objective pressure readings are essential. The STIC® Pressure Monitor from Everis provides fast, clinically supported measurements for both acute and chronic exertional compartment syndrome.
Initially developed by Stryker and now manufactured by Everis, STIC has become a trusted tool for physicians across emergency medicine, orthopedics, and sports medicine. The system uses a side-ported needle to deliver highly accurate results, even in high-stakes situations where diagnosis can’t wait.
STIC enables both single-use and continuous pressure monitoring, providing readings that can be extended up to 24 hours when needed. Its compact, self-contained design supports quick setup and straightforward use, making it easier for clinicians to act fast.
When early intervention matters most, STIC offers the clarity needed to guide treatment and prevent irreversible damage.